The Ultimate Menopause Guide: Symptoms, Stages & Treatments
Overview
- What is Menopause?
- Stages of Menopause: Perimenopause, Menopause, and Postmenopause
- Menopause Diagnosis
- Common Signs and Symptoms of Menopause
- Long-Term Health Considerations Postmenopause
- Treatments for Managing Menopause Symptoms: Medical Options and Supplements
- Nutrition for Menopause: What to prioritise and avoid
- Skincare for Menopause: Skincare solutions and supplements
- Lifestyle Adjustments for Menopause
- Mental Health and Menopause: Tips and Helpful Rescources
- Menopause and Sexual Wellbeing
What is Menopause?
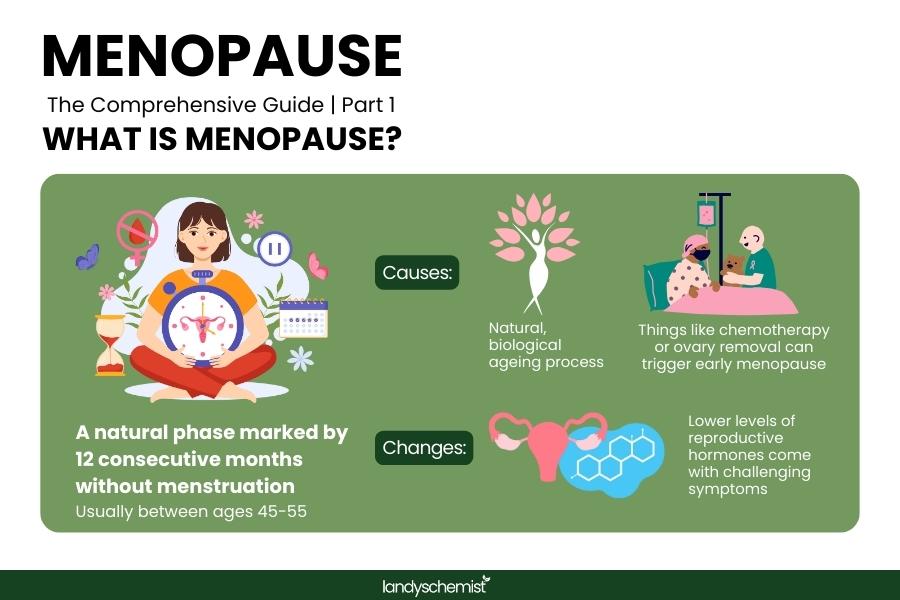
Menopause is a natural phase in a woman’s life marking the end of her reproductive years, defined by 12 consecutive months without menstruation. This milestone typically occurs between the ages of 45 and 55 but can vary widely depending on factors like genetics, overall health, and environmental influences. During menopause, the body undergoes significant hormonal changes, particularly a decline in oestrogen and progesterone levels, which can affect various bodily functions.
While menopause is often associated with ageing, it can also result from medical interventions like surgery to remove the ovaries or cancer treatments such as chemotherapy. These cases, known as induced menopause, can bring about symptoms more abruptly. It’s important to understand that menopause is not a medical condition but a natural transition, one that can come with challenging symptoms such as hot flushes, night sweats, and mood changes. These changes signal the body's adaptation to lower levels of reproductive hormones, impacting everything from bone density to cardiovascular health.
What Are the Stages of Menopause?
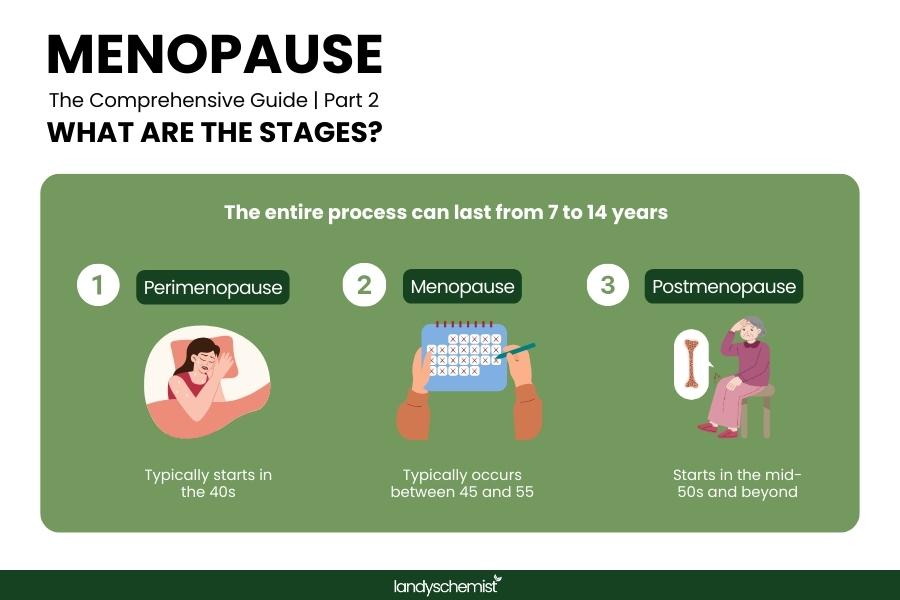
Menopause is a journey that comes in 3 stages, each bringing unique changes to a woman’s body and health. The entire process, from the start of perimenopause to postmenopause, can span anywhere from 7 to 14 years, depending on factors such as genetics, lifestyle, and overall health. A study published in Women's Midlife Health notes that perimenopause is associated with significant biopsychosocial changes, and the duration can vary among women. Here’s an overview of the three key stages of menopause:
Perimenopause (Usually Begins in the 40s):
Perimenopause is the transitional phase leading up to menopause, where estrogen levels begin to fluctuate. This stage can last anywhere from 4 to 10 years, with common symptoms including irregular periods, hot flashes, and mood swings. On average, perimenopause begins around the age of 47.5 years, marking a significant shift in a woman’s hormonal balance. During this time, women may experience a variety of physical and emotional changes as the body prepares for the end of menstruation.
Menopause (Average age 51):
Menopause occurs when a woman hasn’t had a menstrual period for 12 consecutive months. The average age for menopause is 51, although it can vary based on factors like genetics, lifestyle, and other health conditions.
Postmenopause (Starts in the mid-50s and beyond):
Postmenopause marks the phase after menopause, when many women experience a reduction in symptoms like hot flashes. While this phase may bring some relief from earlier symptoms, it also comes with an increased risk of long-term health conditions, including osteoporosis, cardiovascular disease, and weight gain. Importantly, postmenopause is a permanent stage that lasts for the remainder of a woman’s life.
Menopause Diagnosis
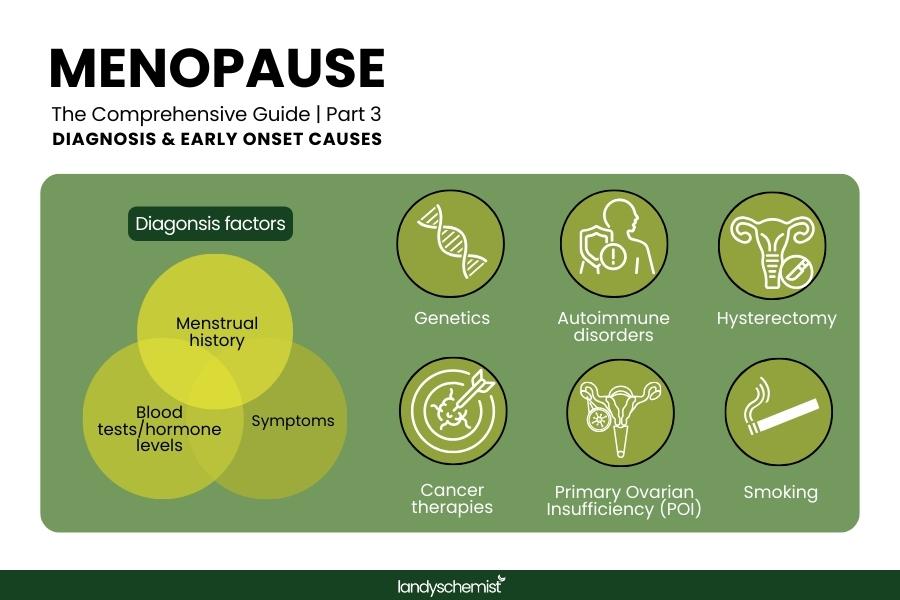
In the UK, menopause is primarily diagnosed based on a woman's symptoms and menstrual history. Blood tests to measure hormone levels, such as follicle-stimulating hormone (FSH) and oestrogen, are generally not necessary for women over 45 with typical menopausal symptoms.
However, for women under 40 experiencing menopausal symptoms, blood tests may be conducted to rule out other conditions and confirm the diagnosis. Additionally, healthcare providers may perform tests to exclude thyroid disorders or other health issues that can mimic menopause symptoms.
What factors cause early menopause onset?
While menopause typically occurs in the late 40s to early 50s, several factors can cause its onset earlier than usual. Early menopause can happen due to:
- Genetics: Family history and specific genetic variants can play a significant role in determining when menopause begins.
- Autoimmune disorders: Disorders like rheumatoid arthritis or lupus can lead to early menopause, often due to inflammation or medication use.
- Smoking: Studies show that smoking is linked to an increased risk of early menopause, with greater intensity, longer duration, and an earlier start age heightening the likelihood.
- Medical treatments: Treatments like hysterectomy (especially with ovary removal) or cancer therapies, such as chemotherapy and radiation, can trigger early menopause.
- Primary Ovarian Insufficiency (POI): A condition where the ovaries stop functioning before the age of 40, often without an identifiable cause.
Signs and Symptoms of Menopause
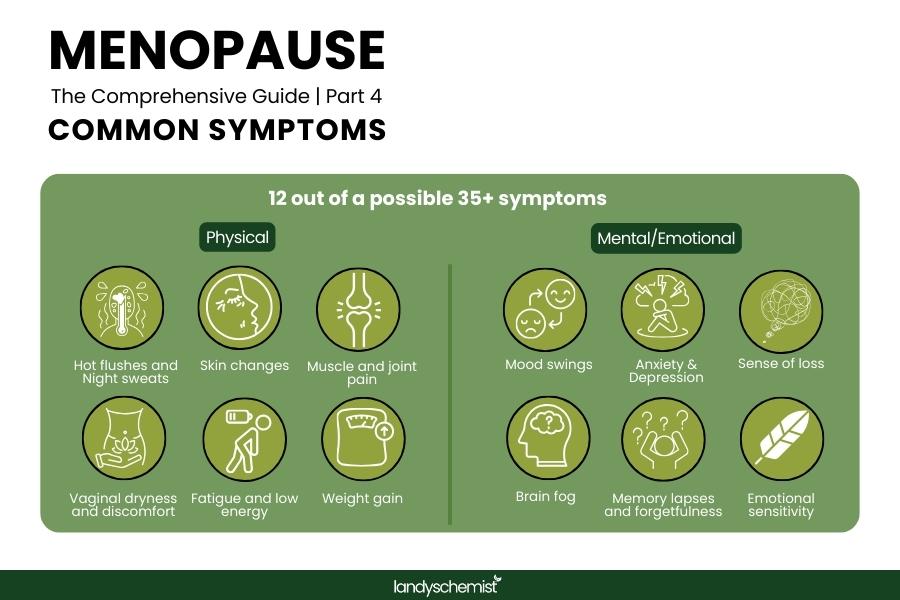
Menopause can bring over 35 recognised symptoms, varying widely in type and intensity among individuals. These symptoms are often grouped into physical and emotional categories, with long-term health risks emerging due to hormonal changes.
Common Physical Symptoms
- Hot flushes and night sweats
- Irregular or missed periods
- Vaginal dryness and discomfort
- Fatigue and low energy levels
- Tingling sensations or numbness in hands and feet
- Muscle and joint pain
- Hair thinning or loss
- Weight gain, especially around the abdomen
- Skin changes, including dryness, acne, and itching
For symptom-specific advice, explore these resources:
- Best Supplements for Menopause Bloating
- Benefits of Sage for Menopause Hot Flushes
- How to Treat Itchy Skin During Menopause
Common Mental and Emotional Symptoms
- Mood swings, irritability, and emotional sensitivity
- Anxiety or feelings of unease
- Depression or a sense of loss
- Brain fog, making it hard to concentrate
- Memory lapses and forgetfulness
Long-Term Health Considerations Postmenopause
Hormonal changes during postmenopause can have lasting effects on health, including:
- Bone Health:Lower oestrogen levels can weaken bones, increasing the risk of osteoporosis and fractures. Read more: Osteoporosis: How To Keep Your Bones Strong & Healthy
- Cardiovascular Health: Hormonal shifts may raise cholesterol levels and heart disease risk. To understand cholesterol read our guide. Natural supplements like red yeast rice and plant sterols may help to manage cholesterol and heart health.
- Weight and Metabolism: Changes in body composition, such as increased abdominal fat, are common postmenopause.
- Cognitive Decline: Reduced oestrogen is linked to memory problems and an increased risk of Alzheimer’s disease.
- Urogenital Health: Reduced oestrogen can weaken pelvic muscles, leading to urinary incontinence or recurrent infections.
Treatments for Managing Menopause Symptoms
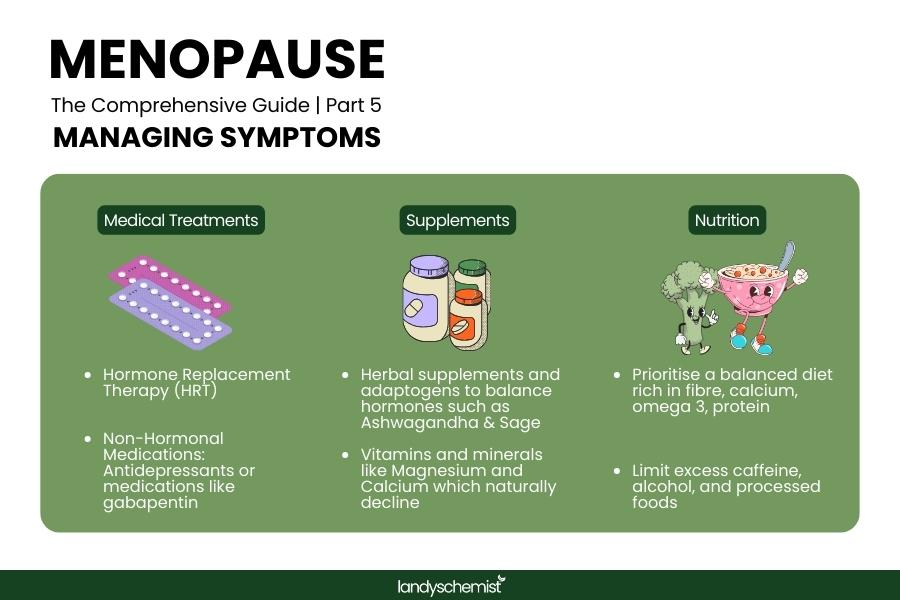
Medical Treatments
- HRT (Hormone Replacement Therapy): A widely used treatment to alleviate hot flushes, night sweats, and vaginal dryness. It also helps reduce bone loss but may increase risks, including breast cancer and blood clots. There are two main types: oestrogen-only HRT (for women who've had a hysterectomy) and combined HRT (oestrogen and progestogen to protect the uterus).
- Non-Hormonal Medications: Options like antidepressants, gabapentin, or vaginal oestrogen can help with hot flushes and dryness, targeting symptoms without affecting overall hormone balance.
Supplements and Alternative Remedies
Many women turn to natural menopause support supplements to manage symptoms. Supplements can be an effective way to manage menopause symptoms naturally.
- Herbal Supplements: Sage extract and black cohosh are popular for managing hot flushes and night sweats, while ashwagandha can help with stress and sleep. Red clover supports hormonal balance.
- Minerals and Vitamins: Magnesium aids mood, sleep, and muscle relaxation, while calcium and vitamin D promote bone health. Vitamin K2 helps direct calcium to the bones.
- Probiotics: Emerging research suggests they may support both digestive and vaginal health during menopause.
Check out these helpful guides:
Nutrition for Menopause
Prioritise
- Calcium-rich foods like dairy, fortified plant-based milk, and leafy greens to support bone health. Read our guide on how Vitamin D3 and D2 work together with calcium to improve bone strength.
- Omega-3 fatty acids from sources like fatty fish, flaxseeds, and walnuts to help manage inflammation and support heart health.
- Fibre-rich fruits, vegetables, and whole grains to aid digestion and manage weight.
Avoid:
- Excess caffeine and alcohol, which can worsen symptoms like hot flushes and disrupt sleep. Opt for caffeine-free options instead such as Bambu Coffee.
- Processed foods high in sugar and refined carbs that may worsen hormonal imbalances and inflammation.
Skincare for Menopause
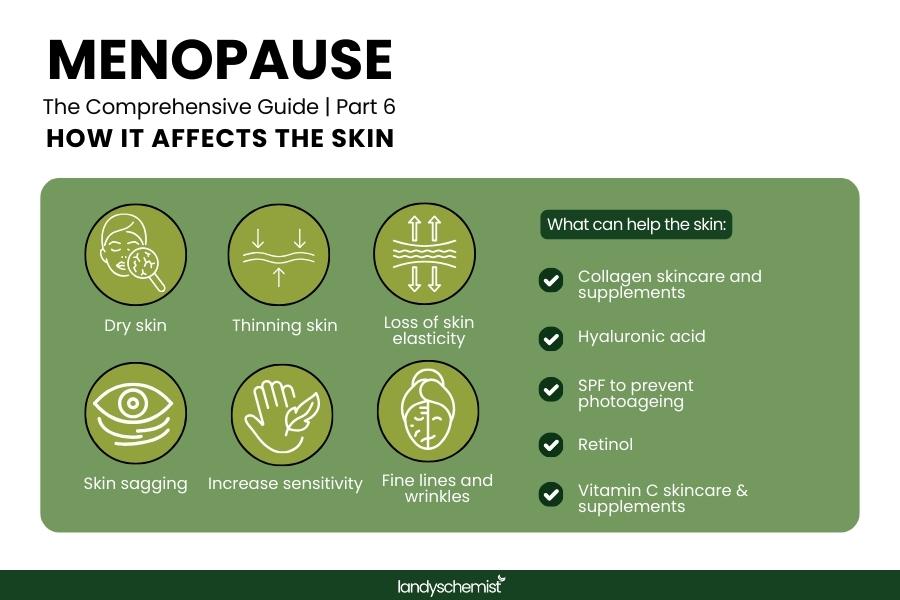
Hormonal changes during menopause can lead to skin changes such as dryness, thinning, and reduced elasticity in the skin. Additionally, a review discusses how estrogen deficiency adversely affects skin functions, including atrophy, wrinkles, hydration, and poor wound healing.
- Hydration: Look for products containing hyaluronic acid and ceramides to replenish moisture and maintain a healthy skin barrier. Targeted dermatological skincare solutions for menopause are also best for addressing skin changes and needs during this phase.
- Collagen support: Topical retinol and peptides, along with collagen supplements, may help firm skin and reduce sagging. Read our detailed collagen guide and how to choose the right collagen for menopause.
- SPF: Daily sunscreen is essential to protect thinning, sensitive skin from UV damage, which can speed up signs of ageing.
- Avoid: Harsh cleansers and fragranced products, as they can irritate sensitive, menopausal skin. Shop cleansers for sensitive skin here.
Further reading:
- Why You Should Always Take Vitamin C With Collagen Supplements
- Best Collagen Supplement for Sagging Skin & Ageing
- Everything you need to know about Menopause
- Photoageing: Why You Should Use SPF To Prevent Signs of Ageing
Lifestyle Adjustments for Menopause
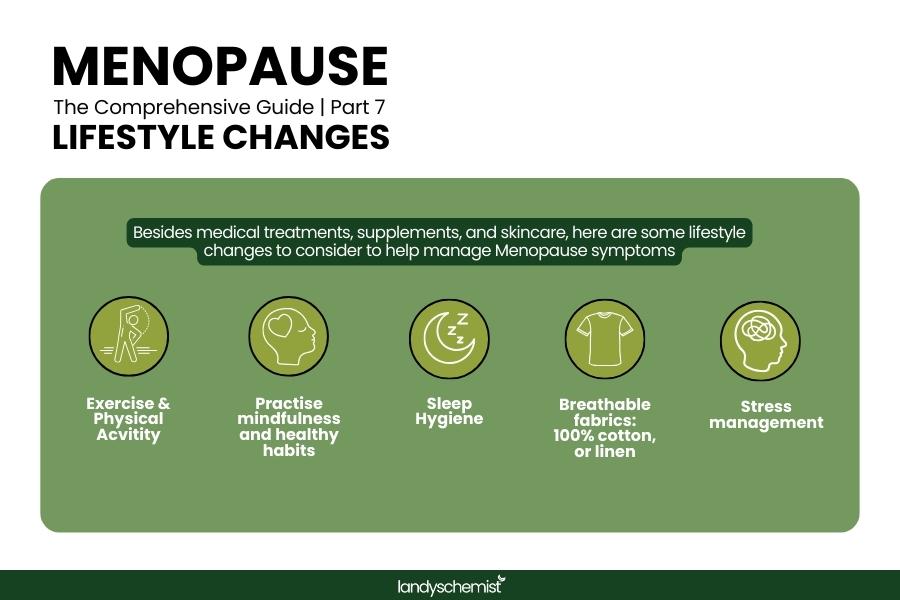
- Exercise: Weight-bearing activities like walking, running, and strength training help strengthen bones. A study found that weight-bearing exercises can help slow bone loss and may even build bone. Whereas Yoga and Pilates can help to improve flexibility, posture, and reduce stress. A systematic review found that pilates exercises can improve quality of life, reduce pain, and enhance flexibility and strength in women with health issues
- Sleep Hygiene: Keep a consistent bedtime and avoid screens before bed to improve sleep quality. Cool bedroom temperatures can help manage night sweats and support restful sleep.
- Stress Management: Practising mindfulness, meditation, and deep breathing techniques can help reduce anxiety and promote emotional well-being.
- Healthy Habits: Avoid smoking, vaping, and excess alcohol consumption to prevent the worsening of menopause symptoms, including mood swings and sleep disturbances.
- Comfortable Clothing: Wear breathable fabrics to stay cool and manage hot flushes effectively, helping you stay comfortable throughout the day.
Menopause and Mental Health
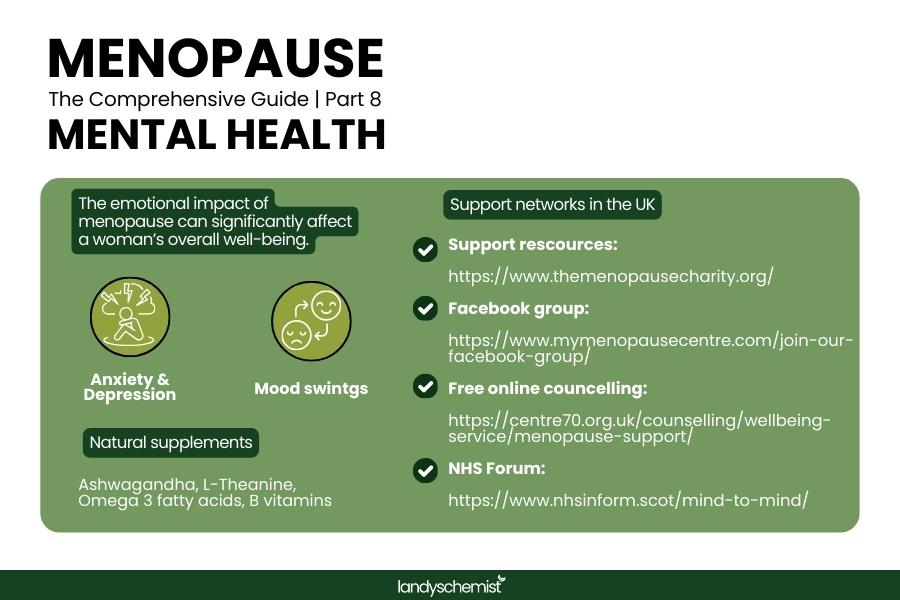
The emotional impact of menopause can significantly affect a woman’s overall well-being. Key mental health concerns include:
- Anxiety and Depression: Hormonal fluctuations during menopause can contribute to feelings of sadness or overwhelm. Herbal supplements like ashwagandha and St. John's Wort, along with amino acids such as L-theanine, have shown promise in alleviating anxiety and depression during menopause. Research indicates that ashwagandha can significantly reduce stress and anxiety, while St. John's Wort is effective for mild to moderate depression, and L-theanine helps improve relaxation and mood regulation. If these feelings persist, professional support is recommended. Visit the NHS forum for more information on how menopause affects mental health and Mental Health UK for resources to support you during this phase.
- Mood Swings: Nutritional supplements, such as omega-3 fatty acids and B vitamins, may help stabilise mood and improve emotional well-being.
- Support Networks: Connecting with online communities or in-person support groups can provide valuable experiences and coping strategies from others going through similar challenges. The Menopause Charity offers trusted support for women experiencing menopausal symptoms as well as free counselling and support groups with Centre70 and My Menopause Centre.
Sexual Wellbeing During Menopause
Sexual health is an important but often overlooked aspect of menopause.
- Vaginal Dryness: Vaginal moisturisers and lubricants can improve comfort. Vaginal oestrogen treatments are also effective for managing dryness. Lady Prelox is a popular natural supplement for improving female pleasure.
- Reduced Libido: HRT and testosterone therapy may help restore libido, but lifestyle changes and open communication with your partner are equally important for a healthy sexual relationship. Read more here: The best supplements for boosting libido.
- Painful Intercourse: Pelvic floor physiotherapy or specialised treatments for vaginal atrophy can alleviate discomfort during intercourse.
Sources
- https://link.springer.com/article/10.1007/s11912-023-01491-5
- https://womensmidlifehealthjournal.biomedcentral.com/articles/10.1186/s40695-020-00052-1
- https://academic.oup.com/edrv/article-abstract/19/4/397/2530801
- https://www.cmaj.ca/content/195/19/E677
- https://www.sciencedaily.com/releases/2019/06/190612110127.htm
- https://www.nia.nih.gov/news/research-explores-impact-menopause-womens-health-and-aging
- https://www.nhsinform.scot/healthy-living/womens-health/later-years-around-50-years-and-over/menopause-and-post-menopause-health/signs-and-symptoms-of-menopause
- https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1518288/full
- https://www.nature.com/articles/s41598-024-59726-9
- https://academic.oup.com/aje/article/187/4/696/4080179
- https://www.ajog.org/article/S0002-9378(19)30588-5/abstract
- https://www.emas-online.org/wp-content/uploads/2020/10/Management-of-urinary-incontinence-in-postmenopausal-women.pdf
- https://www.nhs.uk/conditions/menopause/treatment/
- https://link.springer.com/article/10.1007/s13668-023-00462-3
- https://www.jaad.org/article/S0190-9622(04)02220-0/abstract
- https://link.springer.com/article/10.1007/s13555-020-00468-7
- https://www.health.harvard.edu/staying-healthy/slowing-bone-loss-with-weight-bearing-exercise
- https://www.academia.edu/83400157/Effects_of_Yoga_on_Quality_of_Life_and_Flexibility_in_Menopausal_Women_A_Case_Series
- https://bfpt.springeropen.com/articles/10.1186/s43161-023-00128-9
- https://www.sleephealthjournal.org/article/S2352-7218(24)00090-1/abstract
- https://www.mdpi.com/2813-2998/3/4/47
- https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-016-0325-2
- https://www.cambridge.org/core/journals/acta-neuropsychiatrica/article/effects-of-chronic-ltheanine-administration-in-patients-with-major-depressive-disorder-an-openlabel-study/0373674887BEA9598D911C7B274A3432















